Desperate for Respite
Author: bhi-admin
Desperate for Respite
By Kara Baskin GLOBE CORRESPONDENT MARCH 13, 2015
It’s noon on a dreary winter Friday at the Benson-Henry Institute for Mind Body Medicine at Mass. General Hospital. Cars spray pedestrians
with filthy slush. Sirens squeal, horns screech, people jostle one another on the narrow sidewalks without bothering to look up. But peace and enlightenment may be at hand.
I’m perched on a chair in the office of Dr. Herbert Benson, a twinkly eyed cardiologist who exudes pure beatitude and who has agreed to walk me through the basics of meditation. Benson, 79, is director emeritus of the institute that bears his name. He is the sultan of destressing, a pioneer in mind-body medicine and one of the first physicians to link stress with physical health. Click HERE to read the full article
Study Shows BHI Participants Reduced Doctors Visits by 43%
The core belief of the Benson-Henry Institute (BHI) – that teaching patients mind body approach like meditation and yoga can reduce their stress and improve overall physical health – was proven correct in a preliminary study published this fall in the journal PLOS ONE. The study found that patients who participated in BHI programs reduced their medical visits on average by 43% in the year after taking part.
The study was led by Dr. James E. Stahl of the MGH Institute for Technology Assessment. Dr. Stahl was previously affiliated with BHI and is Chief of General Internal Medicine at Dartmouth-Hitchcock Medical Center.
“Our study’s primary finding is that programs that train patients to elicit the relaxation response – specifically those taught at the BHI – can also dramatically reduce health care utilization,” Dr. Stahl said. “These programs promote wellness and, in our environment of constrained health care resources, could potentially ease the burden on our health delivery systems at minimal cost and at no real risk.”
The relaxation response was first described more than 40 years ago by Herbert Benson, MD, founder and director emeritus of the BHI and a co-author of the study. The physiologic opposite of the well-documented fight-or-flight response, the relaxation response is elicited by practices including meditation, deep breathing and prayer and has been shown to be helpful in the treatment of stress-related disorders ranging from anxiety to hypertension. The paper’s authors note that stress-related illnesses such as anxiety and depression are the third highest causes of health expenditures in the U.S. after heart disease and cancer, which also are affected by stress.
“Studies show that 60 to 90 percent of all medical visits are stress-related. This research proves that we can greatly improve the lives of our patients by integrating stress reduction into our healthcare delivery model,” Dr. Benson said. “This could improve patients’ overall health and reduce healthcare costs dramatically. It’s time to integrate this approach into mainstream medicine.”
Other co-authors of the PLOS One paper include BHI Executive Director Dr. Gregory L. Fricchione, Director of Research John W. Denninger, MD, PhD, Medical Director Darshan Mehta, Researcher Michelle Dossett, MD, PhD, and Roberta Goldman; and Scott LaJoie, PhD, University of Louisville.
“The results are promising and it gives us hope that more rigorous study will bear out the findings of this report,” Dr. Fricchione said. “We are committed to doing the rigorous study because we believe it is so important to the health of our healthcare system.”
Interview with Greg Fricchione
Dr. Fricchione, you are the Associate Chief of Psychiatry at the MGH, Director of its Division of Psychiatry and Medicine, and Director of its world-renowned Benson-Henry Institute for Mind Body Medicine. Tell us more about your clinical and research interests, and what guided you into the field of Mind Body Medicine in particular?
Dr. Fricchione: I’ve been lucky in that I was drawn to a subspecialty called Psychosomatic Medicine and benefitted from training here at MGH in the early 80’s in this field.Psychosomatic Medicine allows you to reside in the borderland between the brain and the body and to stage forays into the land of the body and into the land of the mind across the bridge of the brain, all the while understanding at a very deep level that mind, brain and body are really one country. The age-old mind body question that has vexed philosophers and scientists surfaces in almost every patient you see when you deal with the symptoms and the suffering a psychiatrist deals with on the medical and surgical wards.
So, it is very interesting and it has led to many researchable questions. The catatonic syndrome, for instance, is an amazing natural experiment that has a lot to teach us about the relationship between motivation and movement. Patients who have implantable cardioverter defibrillators are benefited by protection from lethal atrrhythmias but subject themselves to the risk of developing PTSD if their device fires. Researching this will help us understand anxiety disorders. With the dawning of a revolution in our understanding of epigenetics – how the environment can activate and de-activate certain genes – we are discovering ways that mind approaches like meditation, cognitive skills and positive psychology can predispose to a healthier brain and body. I’ve been fortunate to lead the Benson-Henry Institute for Mind Body Medicine here at MGH and we are doing these epigenetic studies as well as clinical and biomarker outcome studies.
What is the Relaxation Response? Tell us about the doctor who had coined the term, and please share with us what you know about its many health benefits.
Dr. Fricchione: Dr. Herbert Benson, a cardiologist, first described the relaxation response. He started as a hypertension researcher and then did the first studies on transcendental meditation back in the late 60’s and early 70’s. He came to the realization that the stress response physiology was counter-regulated by a relaxation response physiology that could be elicited through the use of a variety of meditative techniques, the core features of which are the emptying of one’s mind of everyday concerns combined with a repetitive thought, word, phrase or prayer. When someone is successful in integrating a relaxation response practice into their daily lives, for as little as 10 minutes a day, health can be promoted and stress related illnesses like hypertension, functional bowel diseases, pain syndromes etc. can be prevented. By reducing blood pressure, heart rate, respiratory rate, oxygen consumption, as well as inflammatory response, learning to elicit the relaxation response can help with primary, secondary and tertiary prevention.
Do you think that a ‘mind-body approach’ may be used for dementia prevention and related diseases? If so, what kinds of research and/or clinical programs would you envision for our community?
Dr. Fricchione: There is research to suggest that those with “distress prone personalities” may be more at risk for developing dementia. There is also research implicating a persistent inflammatory response syndrome, perhaps related to amyloid or tau as irritants, in the etiology of Alzheimer’s and oxidative stress in the development of neurodegenerative diseases in general. If reducing stress through relaxation response and enhancing resiliency through mind body approaches plus nutrition, exercise and sleep hygiene, can reduce oxidative stress and the inflammatory response syndrome, perhaps dementia can be prevented or at least delayed by these mind body approaches.
We would like to collaborate with the MGH Dementia Center to put this hypothesis to the test by offering our Benson-Henry Institute approach to the normal elderly and to those with mild cognitive impairment and monitoring them longitudinally for effects on cognitive functioning. In addition given the stress we know that dementia family caregivers experience, we want to begin offering caregiver stress management and resiliency programs to this ever-growing population.
What advice would you give to someone who wants to work in your field?
Dr. Fricchione: Whether you are an internist, a neurologist or a psychiatrist, first become the best traditional clinician you can be. Then focus extra study on how the mind, brain and body are integrated and how this understanding can help you synthesize your practice into what is being called whole person care. Whole person care recognizes the addition of patient self-care as an essential component of health and well being to the traditional components of pharmacotherapy and procedures. Mind body approaches form the foundation of modern self-care. Along the way the engrossing mystery of how the mind, brain and body interpenetrate will be a constant companion.
Lastly, tell us what you like to do during your ‘down-time’? What sustains your enthusiasm and energizes you for all the work that you do for your patients?
Dr. Fricchione: My family is really the most sustaining dimension of my life. I have a wonderful wife of 36 years and 3 great children all living exciting, interesting lives, and also an awesome retired Seeing Eye retriever named Yuma. I like to shovel snow in the winter and swim in the summer and read and hike all year round. And, of course, I try to do my meditation.
Thank you so much for your time, Dr. Fricchione.
Disease Linked to Childhood Stress
According to a new Harvard study that followed 6,700 Britons from age 7 to 45, lifelong distress takes more of a health toll than being stressed in either childhood or adulthood. But if you have to endure distress during just one period, childhood is a more vulnerable time.
Childhood distress may be particularly important because that’s when people are learning how to control their emotions, said Ashley Winning, a postdoctoral research fellow and social epidemiologist at the Harvard TH Chan School of Public Health, who was the first author on the study.
New Program for Kids with Chronic GI Problems
Has your child been diagnosed with a chronic GI condition?
Does your child have Chronic Abdominal Pain, Inflammatory Bowel Disease or Irritable Bowel Syndrome?
Join us for
Resilient Kids: A Mind Body Program
This interactive, engaging, research-validated program gives teens, ages 12-18, the self-care skills they need to reduce physical symptoms and move through life’s physical and emotional challenges with greater resiliency. Your child will learn:
• How stress affects thoughts and feelings
• Meditation methods that can reduce symptoms and improve physical health, such as deep breathing, mindfulness and imagery
• How to foster positive thoughts and attitudes
Enrollment: For more information, or to sign up, please email Rana Chudnofsky at rchudnofsky@partners.org or call 617-643-6068.
Dates, Times and Location:
This eight-session program will begin January 21st 2015. Sessions will be held Wednesdays from 3:30 – 5:00 p.m. at the Benson-Henry Institute,
151 Merrimac Street, 4th floor, Boston, MA.
Cost: $300 per participant
Leadership: This program is led by Leslee Kagan, MS, FNP, and Rana Chudnofsky, Director of the BHI Education Initiative.
Parent Group:
Parents have the option to participate in a separate stress-reduction and resiliency building program while their children’s program is in session. Cost: $200 for one or both parents.
BHI Featured on New England Cable News
An interview with BHI’s Dr. Darshan Mehta about the health benefits of mind body medicine as part of Cancer Awareness Month:Wednesday October 15, 2014
Lovely Testimonial for Successful Aging Program
“It’s taken me most of my life to realize that achievement and competency are not really a path to self-confidence, equanimity and a well-balanced life.
Perfectionism didn’t help me to cover up my ADD blunders and my feelings of unworthiness and shame. Although Alanon has helped me to become a more balanced person with better self-esteem, I have remained anxious and “driven” — a workaholic. My system was wired, and I just couldn’t stop — until a few months ago.
Since starting the Benson-Henry Institute’s Successful Aging program this summer, my meditation practice has deepened and it’s changing me. Ann Webster also offered us several other healing modalities, well integrated into a meaningful sequence. I’ve studied and practiced yoga, tai chi, nutrition, and several other modalities, but having them all integrated made the total greater than the sum of the parts. The best part for me was how much more focused I’m feeling.
I’ve been working at meditating since 1974, but my efforts felt dutiful, were sporadic and didn’t affect me much until this summer. Now I feel greater objectivity and self-awareness. Though I am not yet really focused, there seems to be somebody inside, helping me think more clearly. I don’t feel so overwhelmed by the amount of things I “should” be doing. Sometimes I realize I just don’t want to do a thing. I notice when I’m getting space-y, but I don’t bawl myself out so often. I’m feeling more who I am, and have fewer downs and ups. It seems there’s always something I can do to to help myself feel better. And I don’t have to accomplish some worthy task outside of myself to do it!
Thank you Ann, and all the whole Mind-Body Institute crew.
K.C.
Your Brain: On Yoga
From Shape magazine
October 1, 2014
The stretching feels awesome, and it’s a great excuse to buy more stuff at Lululemon. But devoted yogis know there’s a lot more to yoga than the fashion and flexibility perks. New research shows the ancient practice triggers deep, almost fundamental shifts in the way your brain functions. And the benefits of those shifts can improve your mood and banish anxiety in remarkable ways.
Happy Genes, Happy Brain
You read a lot about stressand its attendant health hazards (inflammation, disease, poor sleep, and more). But your body has a built-in mechanism to counteract stress. It’s called the “relaxation response,” and yoga is a great way to fire it up, shows a study from Harvard Medical School and Massachusetts General Hospital. Among both novices (eight weeks of practice) and long-time yogis (years of experience), just 15 minutes of yoga-like relaxation techniques was enough to trigger biochemical changes in the brains and cells of the downward doggers. Specifically, yoga enhanced activity among those genes that control energy metabolism, cell function, blood sugar levels, and telomere maintenance. Telomeres, if you’re not familiar with them, are caps on the ends of your chromosomes that protect the important genetic material inside. (An oft-used comparison: Telomeres are like the plastic tips that prevent your shoelaces from fraying.) Lots of research has linked long, healthy telomeres to lower rates of disease and death. So by protecting your telomeres, yoga may help your body ward off sickness and disease, the Harvard-Mass General study suggests.
At the same time, those 15 minutes of yoga practice also switched off some genes related to inflammation and other stress responses, the study authors found. (They linked similar benefits to related practices like meditation, Tai Chi, and focused breathing exercises.) These benefits help explain why a large review study from Germany linked yoga to lower rates of anxiety, fatigue, and depression.
Great GABA Gains
Your brain is filled with “receptors” that respond to chemicals called neurotransmitters. And research has linked one type, called GABA receptors, to mood and anxiety disorders. (They’re called GABA receptors because they respond to gamma-aminobutyric acid, or GABA.) Your mood tends to sour and you feel more anxiety when your brain’s GABA activity drops. But yoga appears to boost your GABA levels, according to research from Boston University and the University of Utah. In fact, among experienced yogis, GABA activity leapt 27 percent after an hour-long yoga session, the researchers discovered. Curious to find out whether physical activity was behind the GABA gains, the study team compared yoga to walking indoors on a treadmill. They found significantly greater GABA improvements among the yoga practicers. The yogis also reported brighter moods and less anxiety than the walkers, the study shows.
How does yoga accomplish this? It’s complicated, but the study team says yoga stimulates your parasympathetic nervous system, which is responsible for “rest and digest” activities—the opposite of the fight-or-flight stress responses managed by your sympathetic nervous systems. In a nutshell, yoga seems to guide your brain into a state of safety and security, the study indicates. Most of the research on yoga focuses on types that put a premium on technique, breathing, and blocking out distractions (like Iyengar and Kundalini styles). That’s not to say Bikram and power yoga aren’t as good for your noodle. But the meditative, distraction-blocking aspects of yoga seem to be essential to the activity’s brain benefits, the research indicates.
So grab your mat and your favorite stretchy pants, and put your mind at ease.
You Are Invited!!
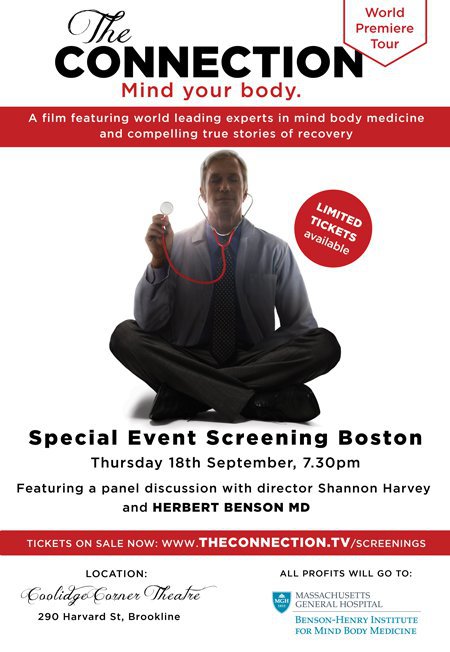
World Premiere Showing of New Film on Mind Body Medicine!
We are pleased to offer you the unique opportunity to attend the Boston Premiere of the film, The Connection that reveals how frontier research is proving there’s a direct connection between our mind and body when it comes to our health. The documentary features a line-up of internationally recognised experts including Dr. Herbert Benson from the Benson-Henry Institute for Mind Body Medicine at Massachusetts General Hospital, as well as compelling true stories of recovery.
After sold-out screenings in Sydney, Melbourne and Worcester, the film will screen in Boston for one night only on its World Premiere Tour.
WHEN: Thursday September 18 at 7:30 p.m.
WHERE: Coolidge Corner Theater, Brookline.
The event will feature an introduction by Dr. Herbert Benson and a Q&A discussion with film director Shannon Harvey (who will be out from Australia).
All profits to benefit BHI.
We recommend purchasing tickets ahead of time. To purchase tickets, click here
Article about Chronic Pain from Pain Medicine News
Communication and Behavior of Physician Important in Managing Chronic Pain
September 2014
Paris—Treatment of chronic pain can be challenging, partly because of the associated problems of depression and anxiety. The patient–provider relationship is one of the key components of managing the psychological aspects of chronic pain, according to experts addressing attendees at the recent 2014 annual meeting of the European League Against Rheumatism.
“Chronic pain is very tricky to treat. For a number of patients, their pain is essentially permanent and ‘untreatable,’ in the sense that it is not going to fully go away. Thus, the treatment can focus on helping patients to be as functional as possible with chronic pain,” said Kevin E. Vowles, PhD, associate professor in the Department of Psychology, the University of New Mexico, Albuquerque, who spoke at the meeting.
The way in which physicians conduct themselves can influence outcomes, he said. Trust is essential, and the physician needs to convey that he or she has the patient’s best interest in mind.
Trust is particularly critical to adherence, said Dr. Vowles, adding that “we know that just telling patients what to do does not work very well.” The physician needs to encourage behavioral change so that patients can adapt their expectations and become comfortable with their experience of pain, he said. For some individuals with chronic pain, this seems to be a viable option, particularly when treatments aimed primarily at pain control have failed to provide benefit or are disrupting functioning.
“Psychology is all about behavior change, which is why it is important in the rehabilitation of chronic pain,” he said. “The ultimate outcome of treatment is not to alter an internal perception but to change the way patients respond to their pain so that they can get on with their lives, ideally in a manner that also allows increased engagement in valued and meaningful activity.”
It is not useful for the patient to try to determine if the pain is “real” or “psychogenic,” he said. ”This dichotomy does not help patients or providers. This is really an outdated concept. For example, in his 1976 book [“Behavioral Methods for Chronic Pain and Illness”], Wilbert E. Fordyce, PhD, outlined many ideas of psychogenic pain that were inaccurate at that time.”
The provider needs to help patients understand that their pain experience will affect their emotions and behavior, and the provider should find ways to help the patient accept the pain and behave so that the pain has as minimal an impact on function as possible.
Some psychological strategies for the treatment of chronic pain include use of acceptance and commitment therapy (ACT), and mindfulness approaches as part of cognitive-behavioral therapy (CBT). These therapies can help patients view their pain in context and make behavioral changes that accommodate the pain, Dr. Vowles said.
“I think treating the psychological components of chronic pain is absolutely critical,” agreed Ellen Slawsby, PhD, director of pain services at the Benson-Henry Institute for Mind Body Medicine at Massachusetts General Hospital in Boston.
Patients with chronic pain have high rates of anxiety and depression, she said. “We have found that 75% have depression, 60% have reduced enjoyment of life, 70% have poor concentration and 75% have sleep disturbances.
“We know pain is exacerbated by the flight-and-fight response [i.e., anxiety]. Paying attention to patients’ psychology will improve symptom control and quality of life,” she said.
Mind–body approaches are important, she noted. “Both ACT and CBT are part of mind–body approaches. Data show that the true relaxation response helps patients with chronic pain get better.”
—Alice Goodman



