Sensitive people’ show heightened activity in empathy-related brain regions
News
Sensitive people’ show heightened activity in empathy-related brain regions
From: Medical News Today
Monday 23 June 2014 – 8am PST
Psychologists at Stony Brook University, NY, suggest that about 20% of the population aregenetically predisposed to be more aware and empathic. Now, in a new study, they explore which regions of the brain are implicated in this. They publish their findings in the journal Brain and Behavior.
Stony Brook’s Elaine Aron, PhD, claims that about 20% of the population are “highly sensitive people” (HSP), who display heightened awareness to subtle stimuli – whether positive or negative – and process information more thoroughly
To investigate whether these traits can be associated with identifiable behaviors, genes, physiological reactions and patterns of brain activity, Dr. Aron and co-author Dr. Arthur Aron, used functional magnetic resonance imaging (fMRI) to examine brain scans of HSP individuals.
The team scanned the brains of 18 married individuals as these participants were shown photographs of smiling or sad faces. The faces either belonged to people who were strangers to the subjects, or they were the faces of their husbands or wives.
The two Dr. Arons describe the team’s findings:
“We found that areas of the brain involved with awareness and emotion, particularly those areas connected with empathetic feelings, in the highly sensitive people showed substantially greater blood flow to relevant brain areas than was seen in individuals with low sensitivity during the 12-second period when they viewed the photos.”
“This is physical evidence within the brain that highly sensitive individuals respond especially strongly to social situations that trigger emotions, in this case of faces being happy or sad,” they add.
Increased activity in brain regions linked with awareness and empathy
When the participants who were classed by the researchers as being HSP saw a photo of their spouse, they exhibited even higher brain activity – with the highest activation of all occurring when a participant viewed images of their spouse smiling.
The areas of this fMRI scan in color represent some of the regions of the brain where greater activation occurs in HSPs compared with non-HSPs.
Image credit: Stony Brook Unirersity
The researchers found that the brain regions exhibiting the greatest activity were those associated with awareness, processing sensory information, action planning and empathetic response – many of which are implicated in the “mirror neuron system.”
A year later, most of the subjects were scanned again, and the researchers observed identical reactions to the previous test.
According to the researchers, the fMRI results confirm that not only are HSPs highly tuned to their environment, but also these heightened awareness and emotional responsiveness traits are intrinsic to this group of humans.
Earlier this year, Medical News Today reported on a study published in the journal Social Cognitive and Affective Neuroscience, where researchers used fMRI to investigate whether witnessing a loved one in distress or experiencing social exclusion causes us to feel physical pain.
The researchers found that both experiencing “social pain” in ourselves and witnessing it in others activates the posterior insular cortex – the brain region linked to the sensory processing of physical pain.
Author Giorgia Silani explained the study’s findings:
“Our findings lend support to the theoretical model of empathy that explains involvement in other people’s emotions by the fact that our representation is based on the representation of our own emotional experience in similar conditions.”
Also, in March, a study published in PLOS One found that the phenomenon of “contagious yawning” is not actually linked to empathy, as was previously thought.
BHI on WGBH’s Greater Boston with Emily Rooney
BHI’s Dr. John Denninger speaks with Emily Rooney on March 13, 2014, about non-pharmaceutical treatment approaches for depression.
Think Yourself Young
http://www.wcvb.com/health/Can-you-think-yourself-young/24518862
From WCVB TV News, Feb 18, 2014
This is a very unusual area of medicine,” said Ann Webster, Ph.D., director of the Program for Successful Aging at Massachusetts General Hospital’s Benson-Henry Institute for Mind-Body Medicine. “These are things people can do for themselves.”
It was at the Benson-Henry Institute that the term “relaxation response” was first coined. It’s an actual physiologic state of deep rest that’s the opposite of the body’s ‘fight or flight’ response.
“This is a time when you restore energy to every cell in your body, and this is also a time when healing can take place,” said Webster.
It may sound far-fetched, but they say it’s grounded in real, cutting-edge science and proven to help people avoid high blood pressure, pain syndromes and even rheumatoid arthritis.
“Take in a deep breath. Hold it … a few seconds, and then let it go,” said Webster. “By the end of the third breath, they’ve already quieted down.”
To turn on the relaxation response, Webster suggests meditation coupled with deep breathing every day for at least 20 minutes, along with:
- Staying fit and eating right
- Keeping a gratitude journal
- Social support
- Staying engaged in life even after retirement
- Getting quality sleep
According to Webster, the number No. 1 barrier to successful aging is obesity.
Mind Body Medicine on the Katie Show
BHI’s Dr. John Denninger and country legend Naomi Judd discuss the health benefits of Mind Body Medicine on Katie Couric’s Katie show.
Half Of A Drug’s Power Comes From Thinking It Will Work
THIS STORY WAS WRITTEN FOR NPR by RICHARD KNOX
January 10, 2014 2:38 PM
When you take a pill, you and your doctor hope it will work — and that helps it work.
That’s not a new idea. But now researchers say they know just how much of a drug’s effect comes from the patient’s expectation: at least half.
When patients in the midst of a migraine attack took a dummy pill they thought was a widely used migraine drug, it reduced their pain roughly as much as when they took the real drug thinking it was a placebo.
“There was no difference between the pharmacology of the drug in reducing pain and the placebo dressed up with a nice word,” study author Ted Kaptchuk tells Shots. “Basically we show that words can actually double the effect of a drug. That’s pretty impressive.”
And if it works when treating migraine headaches, it also might work for a wide variety of other ailments, from asthma to intestinal cramps to back pain, that involve the subjective experience of symptoms.
The findings, in this week’s Science Translational Medicine, have interesting implications for doctors and patients, because what physicians say about a medication appears to have a lot to do with its benefits.
Beyond that, it raises a question of whether drug companies should take subjects’ expectations into account when they test a new drug. (That question may explain why drug-maker Merck helped fund the study, along with the National Institutes of Health.)
The study is the latest in a series that’s helping to decipher the mysteries of the placebo effect. The research is conducted at a newly established Program in Placebo Studies and Therapeutic Encounter at Beth Israel Deaconess Medical Center and other Boston hospitals.
People reported changes in migraine pain after they were given an effective medication called Maxalt or a placebo pill. How the pills were labeled made a big difference.
• No treatment: 15 percent increase in pain.
• Known placebo: 26 percent decrease.
• Placebo labeled Maxalt: 25 percent decrease.*
• Maxalt labeled as placebo: 36 percent decrease.*
• Mystery pill (Maxalt or placebo): 40 percent decrease.
• Known Maxalt: 40 percent decrease.
*Note: These two values are not significantly different statistically.
The group has shown: that placebos rival the effect of active medication in patients with asthma; that even when patients know they’re taking a placebo, they can get relief from the cramps, bloating and diarrhea of irritable bowel syndrome; and that those subliminal suggestions can activate patients’ placebo response.
This time, Kaptchuk and colleagues decided to use migraines to untangle the placebo component of patients’ expectations.
“Migraine is ideal,” Kaptchuk says. “I can’t think of another instance in which a real disease happens and then disappears, and then comes back.” That allowed the group to test patients’ responses against themselves, by watching what happened during seven successive migraine attacks in 66 subjects — 495 attacks in all.
Another advantage is that there’s an effective drug,rizatriptan or Maxalt, that has been shown to work better than placebo pills.
The researchers asked all of their subjects to refrain from taking any medication for two hours after the onset of their first migraine. Then they were given six envelopes, each containing a pill to be taken during their next six migraine attacks.
Two of the envelopes were labeled “Maxalt.” Two indicated that the pill inside could be either Maxalt or a placebo. And two were labeled “placebo.”
Subjects rated their amount of pain two hours after taking each pill.
When subjects took no pills, they reported a 15 percent increase in migraine pain after two hours.
When they took a placebo that was accurately labeled, they reported 26 percent less pain. When they took a Maxalt pill that was properly labeled, they reported 40 percent less pain. And when they took a mystery pill that could have been either a placebo or Maxalt, they also reported a 40 percent decrease in pain.
When subjects took Maxalt that was labeled as placebo, their decrease in pain was statistically no different than when they took a placebo labeled as Maxalt.
“We were surprised that the efficacy of Maxalt mislabeled as placebo was not significantly better than the efficacy of placebo mislabeled as Maxalt,” the researchers write.
One striking thing in the findings is the power of uncertainty. Patients had just as much pain relief when they weren’t sure whether an envelope contained Maxalt or a placebo.
“There’s something going on here that we don’t understand,” Kaptchuk says. “But I think uncertainty engages you in a different way.” It might be analogous, he says, to how doubt can increase the faith of a religious person — it may strengthen the desire to believe.
Kaptchuk says a doctor’s (or researcher’s) manner or words had no effect because patients were only influenced by the words on the pill-containing envelopes.
“What’s exciting is that all we did is change one or two words on an envelope,” the Harvard researcher says. “There was no doctor-patient interaction after the first meeting.”
But in one significant way the placebo didn’t beat the real drug. When the researchers asked patients if they were totally pain-free 2 1/2 hours after taking the pills, patients said Maxalt was almost four times better — 25.5 percent versus 6.6 percent.
That’s consistent with previous placebo studies, Kaptchuk says. For instance, the asthma study showed that asthma inhalants open patients’ airways while placebos don’t. But placebo inhalers reduce patients’ perceived symptoms of asthma.
Being free of migraine pain is a yes/no question, whereas there’s more “wiggle room” in being asked if pain is lessened. “That’s a judgment call,” Kaptchuk says. “Being pain-free is not a judgment call.”
Kaptchuk says the results shouldn’t be seen as undermining the effectiveness of Maxalt. “It’s a really good drug. If I had migraines, I’d take this drug, too,” he says. “But I’d want a physician to understand that every word counts.”
Compassionate Care for Cancer: Why We Need It
The Democrat and Chronicle recently published this essay, written by BHI patient Nila Webster. Read it for her view on the importance of compassionate care, and how it helped her heal and grow.
The Science of Relaxation- Yoga Journal
Curious about the scientific benefits of yoga? Yoga Journal has an interesting current issue, which focuses on scientific research on relaxation techniques such as yoga. For the full link, visit http://www.yogajournal.com/health/2638
Located in one of the best academic medical centers and in one of the most doctor-friendly cities in the country, the Benson-Henry Institute for Mind Body Medicine at Massachusetts General Hospital is well poised to train new doctors to incorporate mind-body techniques into their practice. Its founder and director emeritus, Dr. Herbert Benson, pioneered research on the relaxation response as a powerful antidote to the stress response; he was also one of the first to illustrate that meditation changes metabolism, heart rate, and brain activity as a result of the relaxation response. This commitment to research is still what makes the institute stand out: Benson and his colleagues recently published a landmark study illustrating some of the changes in gene expression that can come from practices that elicit the relaxation response, including meditation and yoga.
Physicians at the institute help treat patients for everything from heart disease to diabetes to infertility. Individual therapeutic yoga instruction is offered as an adjunctive approach for a wide variety of conditions, both physical and mental. Darshan Mehta, the institute’s medical director and director of medical education, says that along with maintaining its commitments to research and patient care, the Benson-Henry Institute is dedicated to educating medical students and residents in integrative medicine. “Boston is famous for training leaders in medicine,” Mehta says. “We need to expose the next generation of doctors to the benefits of mind-body medicine. My hope is that after studying at the Benson-Henry Institute they’ll be able to at least recognize value in it and perhaps add it to their practices in some way.”
Study finds Relaxation Response Triggers Genomic Changes
Meditation, yoga, deep breathing and prayer are all ways to evoke a physiologic state of deep rest known as the relaxation response. New research published in the journal PLOS ONE finds that eliciting this response triggers immediate changes in gene expression that can affect the body’s immune function, energy metabolism and insulin secretion.
The study was a joint effort between the Benson-Henry Institute for Mind Body Medicine at the MGH and Beth Israel Deaconess Medical Center.
“The relaxation response is like the opposite of the fight-or-flight response, which is the body’s natural reaction to stress,” says Herbert Benson, MD, director emeritus of the Benson-Henry Institute and co-senior author of the report. “Previous studies have shown that people experience beneficial changes to their brain while eliciting the relaxation response. And now – for the first time – this study identifies key physiological hubs through which these benefits might be induced.”
The study analyzed the gene profiles of 26 healthy adults who had no experience with the relaxation response. After being taught the relaxation response and following the routine for eight weeks, their profiles were analyzed again. Researchers found significant changes in the expression of several important groups of genes within as little as one relaxation response session. They also found more pronounced changes in those who practiced the response over longer periods of time.
“When you elicit the relaxation response, your energy usage is lowered, your heart beats slower, your muscles relax and your blood pressure decreases. If practiced regularly, it can have lasting effects,” Benson says. “People have been engaging in these practices for thousands of years, and our finding of this unity of function on a basic-science, genomic level gives greater credibility to what some have called ‘new age medicine.’”
Read more articles from the 05/10/13 Hotline issue
1-Day Mind Body Nursing CME – April 9th
The Benson-Henry Institute for Mind Body Medicine (BHI) is pleased to invite nurses and healthcare clinicians to its upcoming continuing medical education program, The Science of Stress and Resiliency: Integrating Mind-Brain-Body Interactions into your Nursing Practice.
The program is offered under the auspices of the Norman Knight Nursing Center for Clinical & Professional Development at Massachusetts General Hospital and will be held Monday, April 9th from 8 AM to 5 PM at Partners Healthcare at Assembly Row, Somerville.
“There aren’t enough drugs or interventions to keep us healthy. Understanding the physiology of stress and the mechanisms and interventions that counter its harmful influence is needed for prevention and treatment of illness and for overall vitality and resiliency. This is an excellent opportunity for nurses to learn how the science of stress affects the brain and body and to develop self-care skills they can teach patients and utilize themselves to build resiliency and reduce burnout,” said course director Peg Baim, MS, NP.
Participants will hear the latest research into the science of stress and how it affects the body at the genomic level, understand how lifestyle behaviors can positively impact health outcomes and build resiliency, build skills in meditation, understand cognitive reappraisal and take part in mind body practices like yoga.
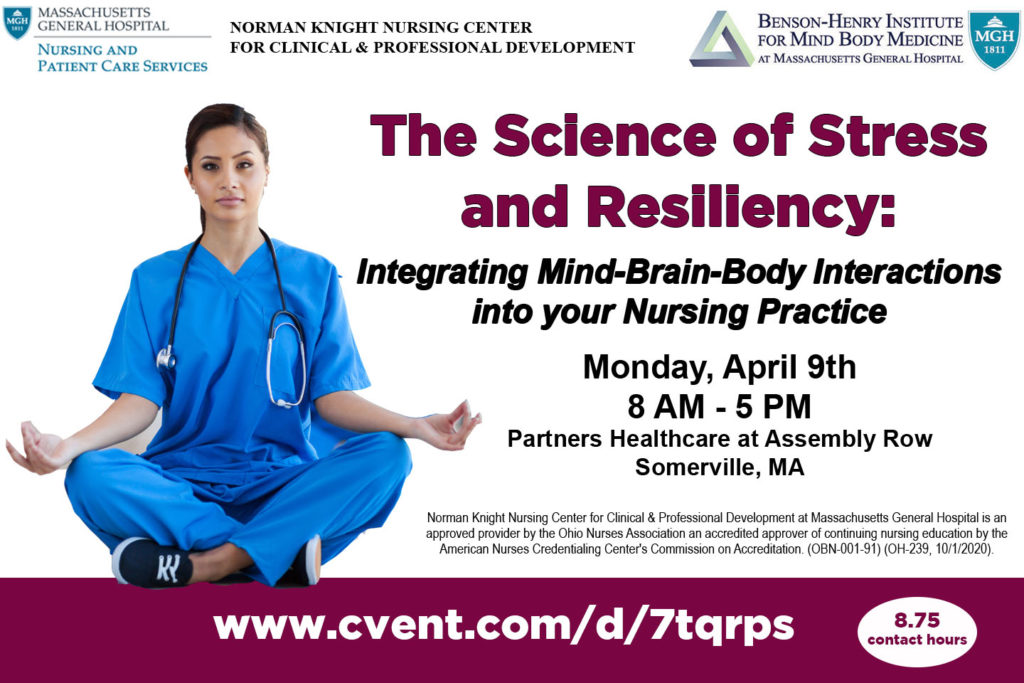
Speakers include BHIS’s Clinical Director of Training, Peg Baim, MS, NP; BHI’s Director of Research, John W. Denninger, MD, PhD; Laura Malloy, LICSW, RYT, Director of Yoga Programs at BHI; and Boston-area nursing leaders Patricia Martin Arcari, PhD, RN, AHN-BC, Program Manager of the Zakim Center for Integrative Therapies at Dana-Farber Cancer Institute; Joanne Rowley, RN, MS, HNB-BC, Clinical Nurse Specialist and Holistic Nurse at MGH Revere; and Women’s Health specialist Leslee Kagan, MS, FNP-BC.
Participation in the course can be applied toward the BHI’s Stress Management and Resiliency Training (SMART) Certification for Healthcare Practitioners program. For more information or to register, visit www.cvent.com/d/7tqrps or email jmeek@partners.org.
Norman Knight Nursing Center for Clinical & Professional Development at Massachusetts General Hospital is an approved provider by the Ohio Nurses Association an accredited approver of continuing nursing education by the American Nurses Credentialing Center’s Commission on Accreditation. (OBN-001-91) (OH-239, 10/1/2020). The Knight Center has awarded 8.75 contact hours.
5 Yoga Poses for Better Sleep
Mandy Oaklander,Heather Jones
Apr 28, 2017
TIME Health
If your goal is sounder sleep, it’s a good idea to try tiring yourself out during the day. Any exercise can do this, of course. But yoga may be the best type for the job.
Not only does yoga offer (often intense) physical activity, but it imparts an extra mind-body benefit. “Yoga helps elicit what we call the relaxation response, which is essentially the physiological opposite of the stress response,” says Laura Malloy, director of yoga programs at Massachusetts General Hospital’s Benson-Henry Institute for Mind Body Medicine. It helps ease any muscle tension you’ve built up throughout the day—even unknowingly—while soothing a racing mind.
For a natural sleep aid, Malloy recommends trying these five yoga poses before bed. Do each pose for six repetitions, or hold them for six cycles of deep breathing.
Click HERE to read the full article



