Your Brain: On Yoga
News
Your Brain: On Yoga
From Shape magazine
October 1, 2014
The stretching feels awesome, and it’s a great excuse to buy more stuff at Lululemon. But devoted yogis know there’s a lot more to yoga than the fashion and flexibility perks. New research shows the ancient practice triggers deep, almost fundamental shifts in the way your brain functions. And the benefits of those shifts can improve your mood and banish anxiety in remarkable ways.
Happy Genes, Happy Brain
You read a lot about stressand its attendant health hazards (inflammation, disease, poor sleep, and more). But your body has a built-in mechanism to counteract stress. It’s called the “relaxation response,” and yoga is a great way to fire it up, shows a study from Harvard Medical School and Massachusetts General Hospital. Among both novices (eight weeks of practice) and long-time yogis (years of experience), just 15 minutes of yoga-like relaxation techniques was enough to trigger biochemical changes in the brains and cells of the downward doggers. Specifically, yoga enhanced activity among those genes that control energy metabolism, cell function, blood sugar levels, and telomere maintenance. Telomeres, if you’re not familiar with them, are caps on the ends of your chromosomes that protect the important genetic material inside. (An oft-used comparison: Telomeres are like the plastic tips that prevent your shoelaces from fraying.) Lots of research has linked long, healthy telomeres to lower rates of disease and death. So by protecting your telomeres, yoga may help your body ward off sickness and disease, the Harvard-Mass General study suggests.
At the same time, those 15 minutes of yoga practice also switched off some genes related to inflammation and other stress responses, the study authors found. (They linked similar benefits to related practices like meditation, Tai Chi, and focused breathing exercises.) These benefits help explain why a large review study from Germany linked yoga to lower rates of anxiety, fatigue, and depression.
Great GABA Gains
Your brain is filled with “receptors” that respond to chemicals called neurotransmitters. And research has linked one type, called GABA receptors, to mood and anxiety disorders. (They’re called GABA receptors because they respond to gamma-aminobutyric acid, or GABA.) Your mood tends to sour and you feel more anxiety when your brain’s GABA activity drops. But yoga appears to boost your GABA levels, according to research from Boston University and the University of Utah. In fact, among experienced yogis, GABA activity leapt 27 percent after an hour-long yoga session, the researchers discovered. Curious to find out whether physical activity was behind the GABA gains, the study team compared yoga to walking indoors on a treadmill. They found significantly greater GABA improvements among the yoga practicers. The yogis also reported brighter moods and less anxiety than the walkers, the study shows.
How does yoga accomplish this? It’s complicated, but the study team says yoga stimulates your parasympathetic nervous system, which is responsible for “rest and digest” activities—the opposite of the fight-or-flight stress responses managed by your sympathetic nervous systems. In a nutshell, yoga seems to guide your brain into a state of safety and security, the study indicates. Most of the research on yoga focuses on types that put a premium on technique, breathing, and blocking out distractions (like Iyengar and Kundalini styles). That’s not to say Bikram and power yoga aren’t as good for your noodle. But the meditative, distraction-blocking aspects of yoga seem to be essential to the activity’s brain benefits, the research indicates.
So grab your mat and your favorite stretchy pants, and put your mind at ease.
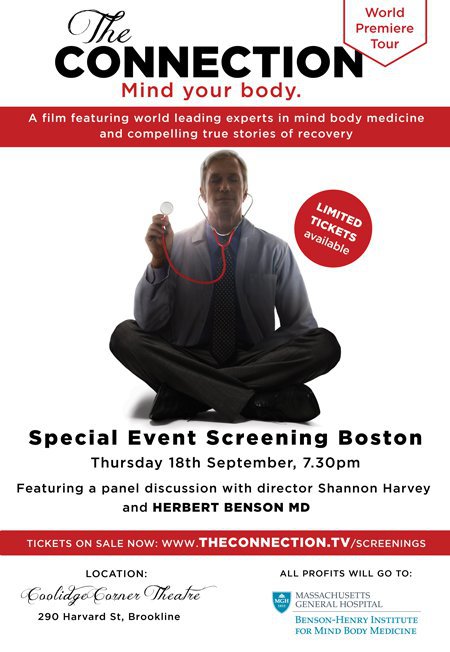
You Are Invited!!
World Premiere Showing of New Film on Mind Body Medicine!
We are pleased to offer you the unique opportunity to attend the Boston Premiere of the film, The Connection that reveals how frontier research is proving there’s a direct connection between our mind and body when it comes to our health. The documentary features a line-up of internationally recognised experts including Dr. Herbert Benson from the Benson-Henry Institute for Mind Body Medicine at Massachusetts General Hospital, as well as compelling true stories of recovery.
After sold-out screenings in Sydney, Melbourne and Worcester, the film will screen in Boston for one night only on its World Premiere Tour.
WHEN: Thursday September 18 at 7:30 p.m.
WHERE: Coolidge Corner Theater, Brookline.
The event will feature an introduction by Dr. Herbert Benson and a Q&A discussion with film director Shannon Harvey (who will be out from Australia).
All profits to benefit BHI.
We recommend purchasing tickets ahead of time. To purchase tickets, click here
Article about Chronic Pain from Pain Medicine News
Communication and Behavior of Physician Important in Managing Chronic Pain
September 2014
Paris—Treatment of chronic pain can be challenging, partly because of the associated problems of depression and anxiety. The patient–provider relationship is one of the key components of managing the psychological aspects of chronic pain, according to experts addressing attendees at the recent 2014 annual meeting of the European League Against Rheumatism.
“Chronic pain is very tricky to treat. For a number of patients, their pain is essentially permanent and ‘untreatable,’ in the sense that it is not going to fully go away. Thus, the treatment can focus on helping patients to be as functional as possible with chronic pain,” said Kevin E. Vowles, PhD, associate professor in the Department of Psychology, the University of New Mexico, Albuquerque, who spoke at the meeting.
The way in which physicians conduct themselves can influence outcomes, he said. Trust is essential, and the physician needs to convey that he or she has the patient’s best interest in mind.
Trust is particularly critical to adherence, said Dr. Vowles, adding that “we know that just telling patients what to do does not work very well.” The physician needs to encourage behavioral change so that patients can adapt their expectations and become comfortable with their experience of pain, he said. For some individuals with chronic pain, this seems to be a viable option, particularly when treatments aimed primarily at pain control have failed to provide benefit or are disrupting functioning.
“Psychology is all about behavior change, which is why it is important in the rehabilitation of chronic pain,” he said. “The ultimate outcome of treatment is not to alter an internal perception but to change the way patients respond to their pain so that they can get on with their lives, ideally in a manner that also allows increased engagement in valued and meaningful activity.”
It is not useful for the patient to try to determine if the pain is “real” or “psychogenic,” he said. ”This dichotomy does not help patients or providers. This is really an outdated concept. For example, in his 1976 book [“Behavioral Methods for Chronic Pain and Illness”], Wilbert E. Fordyce, PhD, outlined many ideas of psychogenic pain that were inaccurate at that time.”
The provider needs to help patients understand that their pain experience will affect their emotions and behavior, and the provider should find ways to help the patient accept the pain and behave so that the pain has as minimal an impact on function as possible.
Some psychological strategies for the treatment of chronic pain include use of acceptance and commitment therapy (ACT), and mindfulness approaches as part of cognitive-behavioral therapy (CBT). These therapies can help patients view their pain in context and make behavioral changes that accommodate the pain, Dr. Vowles said.
“I think treating the psychological components of chronic pain is absolutely critical,” agreed Ellen Slawsby, PhD, director of pain services at the Benson-Henry Institute for Mind Body Medicine at Massachusetts General Hospital in Boston.
Patients with chronic pain have high rates of anxiety and depression, she said. “We have found that 75% have depression, 60% have reduced enjoyment of life, 70% have poor concentration and 75% have sleep disturbances.
“We know pain is exacerbated by the flight-and-fight response [i.e., anxiety]. Paying attention to patients’ psychology will improve symptom control and quality of life,” she said.
Mind–body approaches are important, she noted. “Both ACT and CBT are part of mind–body approaches. Data show that the true relaxation response helps patients with chronic pain get better.”
—Alice Goodman
Managing Back-to-School Stress
Hans Selye, a pioneering Hungarian scientist who was a pioneer in modern stress research, was quoted as saying, “It’s not stress that kills us, it is our reaction to it.”
Today, 75 years after he made that statement, it rings as true as ever. And nowhere is it more challenging to find an effective response to stress than among our kids.
An annual survey by the American Psychological Association (APA) in 2013 identified today’s teens and young adults (age 18-33) as the “most-stressed generation” in the United States. Nearly half of the teens surveyed said that they had stress but couldn’t manage it. Another recent survey of seventh graders found that only 36 percent of students agreed with the statement, “I am happy with my life.”
Heading into the school year can be a particularly stressful time for kids, and a great time to start implementing long-term strategies to improve our and our kids’ ability to cope with stress.
Here are a few simple but important ways you can help your children and yourself to have a successful and less stressed start to the school year.
- Start the school sleep schedule early. A good night’s sleep is one of the most important stress reducers, as sleep helps to manage hormone levels, maintain a healthy body weight, and maintain and grow muscle tissue. Start the school sleep routine a week or two before the first day of school, to ease the transition from late summer nights. Getting into a good sleep routine will work best if you create a consistent bed time, keep away from the screen for at least 2 hours before bedtime, and do some type of winding-down exercises before bed such as prayer and other forms of meditation, gentle stretching, playing soothing music, or taking a bath.
- Be as prepared as possible. If you have school-age children, visiting the school can help them feel more comfortable and excited about returning. Find out who their classmates are, and if possible, ensure they have at least one friend in their classroom. Shopping for school supplies and other necessary items can be a fun transition ritual that has the important benefit of bringing a sense of control to a new situation. Along these lines, you can extend the preparation ritual by setting up a study area for your child. A quiet, organized space that is designated for schoolwork will encourage commitment and follow-through to the homework routine.
- Talk about it, and stay positive. Another great way to prepare for the coming year is to simply talk to your child about their feelings. Find out what’s making them anxious; validate those feelings and work together to come up with potential solutions.If possible, carve out some quality time before school starts to reminisce about the joys of summer and any worries about the new school year.You might create a night-before-school special meal; showing enthusiasm yourself is sure to spread to your kids, turning their nervous energy into excitement. This may be especially important to do on Sunday evenings, which is when kids most often become stressed about school the next day. As a parent, you send your children an important message by assuring them that they can get through a transition, even if it’s hard.
- Help your child set realistic priorities for school and outside activities. Talk to them about finding a balance among discipline, self-challenge, and enjoyment. Maybe they don’t need to do three sports, or maybe they need encouragement to try something new. Establishing a successful schedule will go a long way to reducing stress. Part of this schedule should include down time, where nothing is scheduled and you have the opportunity to connect with your child. That relaxed connection can be a tremendous stress relief.
Finally, be a role model. In this stress-filled world, it is valuable for us to show our children how to counteract stress. Let them see you taking a few minutes to sit still while you concentrate on your breathing. Tell them about your own commitment to create a less stressful year.
In many ways school is the testing ground for a lifetime of challenges and opportunities that your child will face throughout his or her life. Providing children with a toolbox of ways to reduce their worry early in life can go a long way to promoting a lifetime of well-being.
Osher Center to Host Integrative Medicine Research Forum
On November 3rd, 2014, the Osher Center for Integrative Medicine Research will host its inaugural Integrative Medicine Research Forum. BHI Medical Director Darshan Mehta, MD, MPH, will be presenting at this free event, the first-of-its kind in-person gathering, bringing together the rich and diverse Boston-wide network of experts and practitioners with interests in integrative medicine research. The submission of IM Research Abstracts are invited for presentation at the Forum.
Schedule:
12:15 pm – 6:30 pm Half-Day Symposium
Keynote Speakers:
Professor Albert Laszlo Barabasi, Robert Gray Dodge Professor of Network Science and Distinguished University Professor at Northeastern University.
David King, Founder, Exaptive, Inc.
Guest Speakers from:
- The Osher Center for Integrative Medicine
- Benson-Henry Institute for Mind Body Medicine
- Zakim Center for Integrative Therapies
- Cheng-Tsui Integrated Health Center, and
- Representatives from Boston University, Tufts Medical School and Cambridge Health Alliance
To register, please visit oshercenter.org
Top Quotes after last year’s CME Conference
There is still time to register and join world-renowned experts and workshop leaders at Benson-Henry Institute’s fall CME course, The New Science of Resiliency and its Clinical Applications.
Past attendees consistently rank this 4-day course as one of Harvard’s best CME programs. Here are just a few of the many positive comments we received after last year’s course:
“It is rare that I take away as many concepts, techniques or interventions as I am doing today.”
“A powerful blend of research, heart, experience and love of mind body work.”
“Topics extremely thought provoking.”
“Excellent conference both in content and presenter’s delivery”
“Wonderful. Fed my soul.”
This year, we are honored to welcome Bruce S. McEwen as our keynote speaker. The author of over 600 peer-reviewed articles, Dr. McEwen is unparalleled in his contributions to the scientific understanding of the influence of stress on health and illness.
Participants will come away with
• a strong understanding of the scientific foundation of mind body mechanisms and health
• insights into the latest and most exciting brain imaging and genomic research, as well as the role of mind body medicine in public health.
• The ability to apply mind body interventions with their patients
• Techniques to avoid provider burnout
Partner’s affiliates receive a 30 percent discount!! For more information and to register, visit http://www.hms-cme.net/341983/ or call Jill Buchanan at 617-643-6043.
Stressed Out- Who, Why and How
From NPR’s show, The Exchange with Laura Knoy
From major challenges like chronic illness or financial problems to minor annoyances like traffic jams or inconsiderate neighbors, stress affects us all. For some, it can be overwhelming, while others find ways to cope and even use it to their advantage. In connection with the NPR series on this topic, we’re exploring the latest thinking on stress.
Click HERE
Summer 2014 MGH Hotline Article
Mind Over Matter
When Joanne Ring’s husband passed away three years ago, she found herself working through a grief process that became nearly impossible to manage. Raising four young boys and working fulltime as an ICU nurse only added to her stress and anxiety. Although her primary care physician offered medication to help her cope with her anxiety, Ring felt there was a better option.
She turned to the MGH Center for Community Health Improvement in Charlestown, which works with the MGH Wellness Center and Benson-Henry Institute for Mind Body Medicine (BHI), to offer group mind-body intervention (MBI) as a plausible option for treating anxiety and depression.
The eight-week MBI group is provided at MGH community health centers in Revere and Charlestown by licensed clinical social workers trained in MBI at BHI. The groups meet once weekly for 90 minutes. The program includes teaching methods eliciting the relaxation response using a variety of techniques, along with promoting adaptive cognitive practices, such as optimism and acceptance; promoting healthy lifestyle behaviors, such as recommendations for nutrition, exercise, and restorative sleep; and building social support.
“The BHI Wellness Center conducted a retrospective study looking at the medical records of 124 patients who had participated in the MBI groups for anxiety and depression,” says Kathleen Miller, RN, PhD, director of the BHI Wellness Center, and a principal author of the study.
“Participants in our study showed improvements in symptoms of depression and anxiety, as well as decreases in perceived stress. Based on this, we think the group MBI may be a good resource for community health center providers to recommend as adjunctive treatment for anxiety, depression and stress.”
Ring says, “If I hadn’t learned some of the strategies channeling the relaxation response, I likely would have ended up on medication – a route I really didn’t want to take. The tools I’ve learned to manage my stress and anxiety, coupled with positive lifestyle alterations, have truly changed my life for the better.”
The study, entitled “The Effectiveness of a Community-based, Mind-Body Group for Symptoms of Depression and Anxiety,” was published in the summer 2014 issue of Advances in Mind-Body Medicine.
People In the Field…
Upcoming CME Keynote Speaker Feature
Bruce McEwen- Unparalleled depth and breadth in Stress Research
The Benson-Henry Institute is honored to welcome Bruce S. McEwen, PhD, as keynote speaker for its CME Course, The New Science of Resiliency and its Clinical Applications, which will be held September 16-19 in collaboration with Harvard Medical School. For more information, please visit http://bensonhenryinstitute.org/professional-training/live-cme.
For more than 40 years, Dr. McEwen has studied the mechanisms and impact of stress on humans. McEwen’s depth of experience in studying stress hormones and the brain is unequaled, and his work has far-reaching implications for understanding the impact of stress on human health in general.
Among his remarkable accomplishments, McEwen has:
* Contributed heavily to a new understanding of how the brain changes in structure and function during development and in adult life.
* Helped draw distinctions between good or adaptable forms of stress and toxic stress.
* Expanded our understanding of allostatic load, a widely used term that explains how stress systems that help the body survive can cause problems when overworked.
* Significantly contributed to understandings of gender differences in stress effects.
* Expanded awareness of how circadian disruption, arising from shift work, jet lag, and sleep deprivation, can affect brain function and behavior.
McEwen is the author or co-author of more than 900 scientific papers, and co-author of two books for the lay public. His is currently the Alfred E. Mirsky Professor and Head of the Harold and Margaret Milliken Hatch Laboratory of Neuroendocrinology at The Rockefeller University. He is also involved with the National Scientific Council on the Developing Child, which investigates how early life stress can be ameliorated to minimize its lifelong consequences.
The Health Burden of Stress
LIVE WEBCAST: Wednesday, July 9, 2014, 12:30-1:30pmET.
Do you have resources to share to help manage stress to improve health? During the webcast on July 9, we will invite you to Tweet your ideas using hashtag #BurdenofStress.
You also can Tweet questions for the panelists before or during the live webcast to @ForumHSPH. Or, e-mail them to theforum@hsph.harvard.edu. We’ll also be conducting a live chat on this web page during the live webcast. For many of us, stress is an omnipresent and frequently overwhelming factor of day-to-day life. As we begin to better understand its toll on our health, this Forum at the Harvard School of Public Health event – in connection with a new poll by HSPH, the Robert Wood Johnson Foundation and NPR – will share the story of stress as perceived by many Americans. What are the biggest sources of stress? How can it affect our health? And what can we do in our homes, workplaces and communities to help us manage stress and to live calmer – and healthier – lives?
Presented in Collaboration with the Robert Wood Johnson Foundation and NPR
Background Articles
- The Robert Wood Johnson Foundation
- Harvard School of Public Health Opinion Research Program
- NPR
Science Section - Benson-Henry Institute for Mind Body Medicine
MGH - Poll: The Burden of Stress in America
NPR/Robert Wood Johnson Foundation/Harvard School of Public Health



